The Scales Have Tipped: Why Weight Watchers' Demise Signals a Need for Stigma Free Healthcare
- Nutriri Weight Neutral
For decades, Weight Watchers (WW), now WW International, has been a dominant force in the diet industry. Its focus on points systems and weekly weigh-ins promised a path to a healthier body. However, recent reports indicate the company is facing significant financial struggles, with talks of potential bankruptcy - with rumoured debts of $1.4 billion.
VCSE Nutriri believes such decline as not simply a business downturn; but a reflection of a broader shift in understanding around health, weight, and the damaging physical and mental impacts of weight-centric approaches.
The traditional weight change model, exemplified by many businesses like WW, operates on the premise that weight is the primary determinant of health and that individuals can and should actively strive for weight reduction through surveillance and restriction. This approach, however, overlooks crucial evidence regarding the ineffectiveness of long-term weight change for many and the significant harm caused by weight stigma.
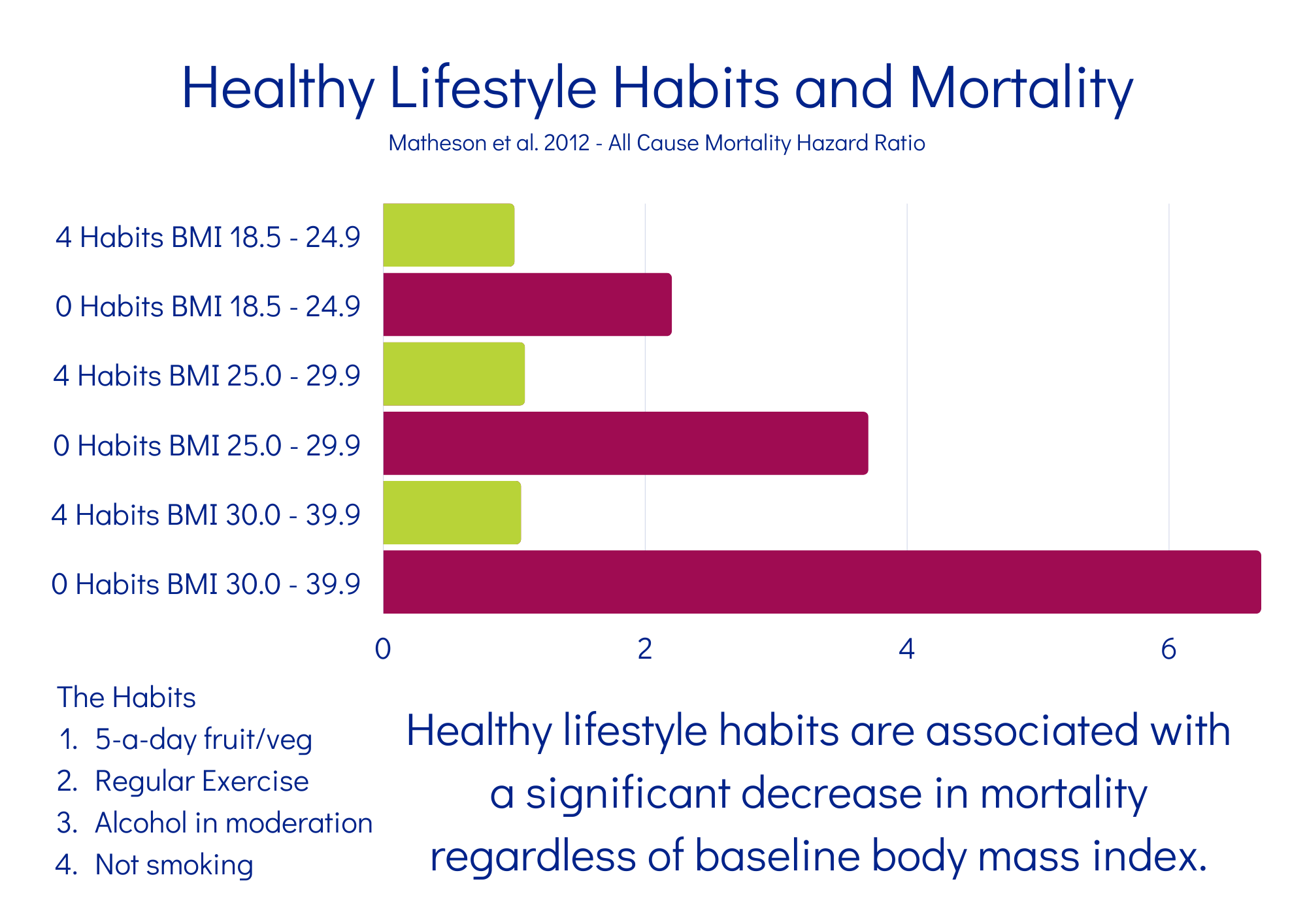
Long term studies (https://www.jabfm.org/content/25/1/9) over the last 2 decades prove that...
it is beneficial behaviours sustained over time that influence health - independent of body size
The Fallacy of Weight Surveillance and its Detrimental Effects:
The emphasis on regular weighing and the categorisation of humans based on metrics like Body Mass Index (BMI), body composition, waist/height ratios have had unintended and harmful consequences. Constant surveillance and focus on body size can lead to:
Reduced Cancer Screenings: Anxiety and internalised stigma can create significant barriers to healthcare access. Individuals in larger bodies may avoid medical settings due to fear of judgement or negative experiences related to their weight. This avoidance can lead to lower rates of crucial preventative screenings like mammograms, cervical screenings and prostrate examinations, potentially resulting in later diagnosis and poorer outcomes for cancers.
Lowered Trust and Engagement in Health Systems: When healthcare interactions are dominated by weight-focused advice and stigmatising language, trust between patients and providers erodes. People in larger bodies may feel unheard, blamed, or dismissed, leading to decreased engagement with healthcare services overall. This can result in delayed or forgone treatment for various health concerns, not just those perceived to be weight-related.
Increased Psychological Distress: The constant pressure to change weight and the internalisation of negative societal messages about higher weight contribute to anxiety, depression, and disordered eating patterns. This psychological burden can have significant negative impacts on overall health and well-being.
The Rise of Stigma-Informed Systems and Social Prescribing:
The decline of weight-centric models like WW presents an opportunity to move towards more holistic and stigma-informed approaches to health. Size acceptance frameworks, such as Health at Every Size (HAES®), recognise that health exists across the weight spectrum and prioritise health over body size.
VCSE Nutriri's tag #MeasureHealthNotWeight is an urgent call - with a robust plan - to reduce health inequalities and rebuild trust in our health systems.
These frameworks advocate for:
Respect for Body Diversity: Acknowledging and valuing the natural variation in body size and shape - think dog breeds but for humans! watch ASDAH's Poodle Science https://youtu.be/H89QQfXtc-k?si=QClsob6msszo3lbr
Prioritising Beneficial Behaviours: Focusing on sustainable behaviours that support physical, mental, and social well-being for all individuals, regardless of size. This includes equitable access to nutrient rich foods, welcoming and safe movement spaces and sports, stress management, and social connection.
Ending Weight Discrimination: Working to dismantle the systemic biases and prejudices faced by people in larger bodies in all areas of life, including healthcare.
Social Prescribing Hubs: A Stigma-Informed Alternative:
Social prescribing offers a promising model for facilitating stigma-informed care. These hubs connect individuals with non-medical sources of support within their communities, addressing the core determinants of health such as social isolation, financial insecurity, and lack of access to resources. Instead of focusing on individual weight change, future social prescribing hubs can empower people to engage on their own terms:
Build Social Connections: Participating in community groups and activities reduces loneliness and fosters a sense of belonging.
Meaningful Activities: Access to arts, culture, gardening, and volunteering can improve mental and physical well-being.
Underserved Needs: Support with housing, employment, and financial issues can reduce stress and improve overall health.
Access Health Information and Support: In a non-stigmatising environment that promotes trust and open communication.