Instead of...
"Slimming" Clubs - let's have Neighbourhood Health Hubs
Are you still trying to 'solve obesity'?....
All forms of stigma intersect. They carry similar health impacts. Discrimination based on race, gender, sexuality, size and other characteristics create layers of disadvantage. Each layer compounds the harm. This case study focuses mostly on weight stigma. It explores its specific impact. It also reveals its connection to wider systems and opportunities for change.
VCFSE (Voluntary Community Faith Social Enterprise) Nutriri has been built by volunteers sharing their lived and living experiences of ‘weight talk’ in healthcare, family and community. We set out to listen to the lived and living experiences of the NHS workforce and citizens to research and improve access and engagement with healthcare, food and movement without surveilling weight.
Many people delay or withhold from engagement through anticipated ‘weight talk’ and internalised stigma. Weight is often a correlatory presentation alongside long term health conditions, making ‘weight talk’ a significant contributor to multiple disadvantages and healthcare inequalities.
The impact of ‘weight talk’ in the consultation room and beyond…
Shaw/Meadows 2022 “weight stigma among healthcare providers is linked to healthcare avoidance in patients, including under-utilisation of preventive health care and screening; evidence consistently demonstrates that stigma is more likely to lead to increased allostatic load, higher prevalence of chronic diseases, and further weight gain, independent of BMI”
Consider a patient with higher weight and a long term health condition who has previously had their weight highlighted as the main cause or contributor to their condition and symptoms. Perhaps only prescribed weight change as a treatment and had the health condition overlooked. The patient - if they initially attend at all - often leave the consultation less engaged with trust eroded, and no clear plan to collaborate on their health.
Weight stigma does not operate in isolation; it intersects with other biases, creating a compounding effect that further marginalises individuals. The complex interplay between weight stigma and multiple disadvantages extend to socioeconomic factors. Individuals who experience poverty often have less access to nutritious food, safe exercise spaces, elevated stress and more pressing priorities, further perpetuating the cycle of disadvantage.
The challenge is to improve access and engagement - without surveilling weight (regardless of personal weight change intentions) - to determine whether working weight neutrally/inclusively is beneficial to individuals and services alike. For example ‘Does weight neutral messaging increase participation in services?’ and ‘Does stopping measuring weight rebuild trust, elevate engagement and raise population health?’
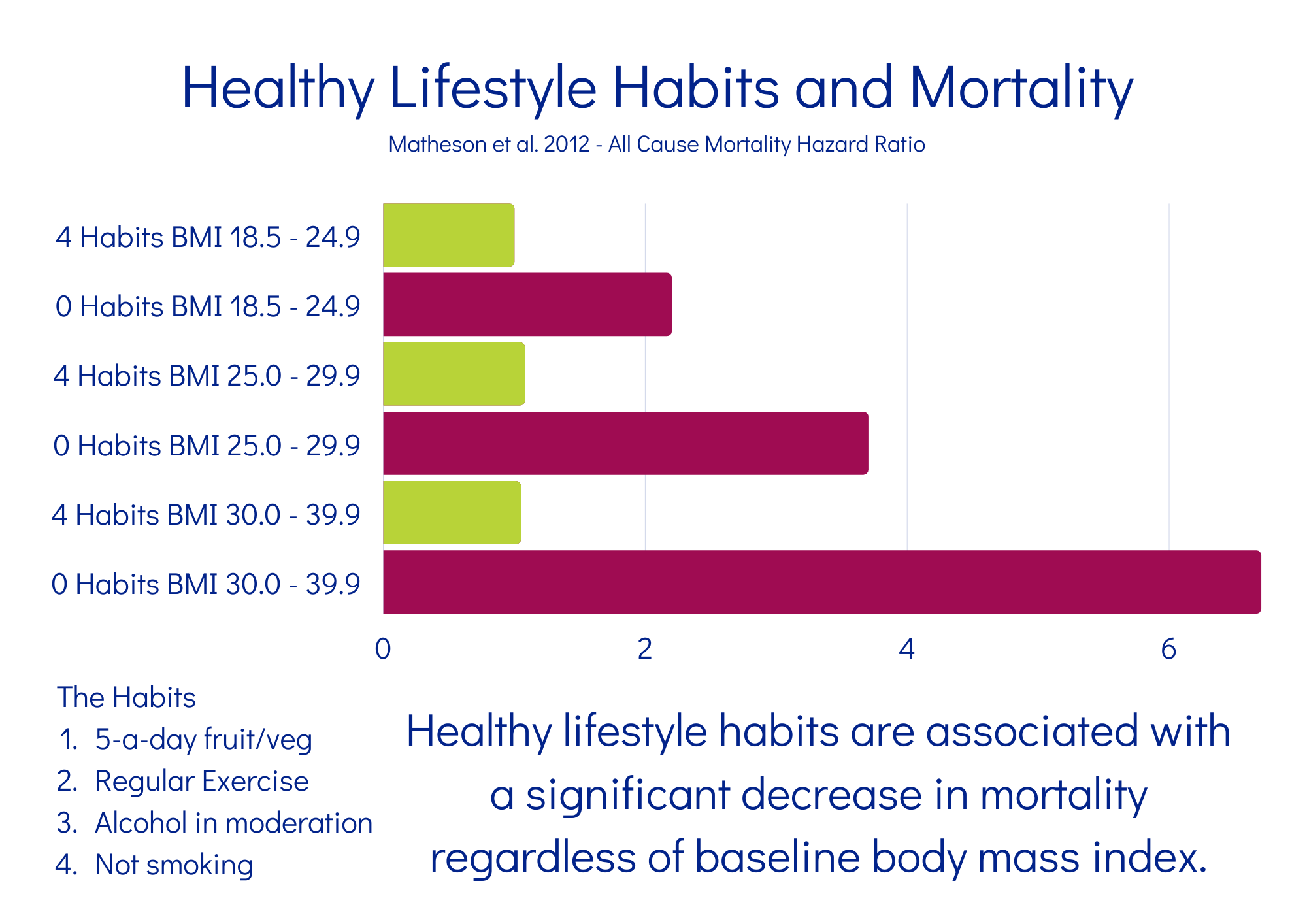
Addressing weight stigma and its intersection with multiple disadvantages requires an holistic approach that reduces individual blame, and focuses on cohesive action, within the community, and shifts societal biases. It is crucial to recognise that changes in physical activity, balancing nutrition, alcohol consumption, and smoking cessation can significantly improve public health outcomes, independent of weight change. A study by Matheson 2012 clearly demonstrates that it is behaviours sustained over time that bring health, and not weight change itself.
Since 2015, volunteers have been meeting and sharing their experiences of ‘weight management’ and ‘diet culture’ to enable us to co-create...
One for workforce Weight Neutral Training and one for citizens Food & Body Ease. These are facilitated on this Co-Learning Hub where the co-creation continues with each participant’s lived experience included and valued. We operate a ‘no wrong door’ approach where a co-learner may initially engage through workforce training but also go onto the Food & Body Ease pathway for their personal focus, and sometimes vice versa.
P (Population) - Healthcare workforce who’s role includes talking about weight.
I (Intervention) - Weight bias awareness intervention - Nutriri Weight Neutral Training - Curriculum: What is Weight Neutral?, What is Weight Stigma?, Health Inequalities and Determinants, What to Measure Instead, Resources and Further Research - self paced digital platform co-learning style.
C (Comparison) - Healthcare workforce who do not receive the above weight inclusive intervention.
O (Outcome) - Stigma Informed Systems; Reduction in explicit and implicit weight bias amongst the healthcare workforce; improved attitudes and beliefs about patients with higher weight; improved access to, and engagement with, general healthcare. Improved patient activation measure; increased length of engagement in beneficial behaviours; Increasing equity and reducing harms and inequalities as we move away from individual blame and reliance on weight change often mis-used as a health metric.
P (Population) - Adults seeking "weight management" support; adults withholding from healthcare through perceived, or actual, risk of weight stigma; adults with a history of weight cycling or general disordered eating. Adults with co-occurring health needs.
I (Intervention) - Participation in the Nutriri Food and Body Ease course and community - support to find enjoyable movement, general disordered eating recovery, body neutrality, intuitive eating, group hypnotherapy (if not contraindicated), group coaching.
C (Comparison) - Adults referred to current weight KPI focused activities.
O (Outcome) - Prolonged engagement in equitable beneficial behaviours in the absence of weight KPI’s; increases in body satisfaction; decreases in negative mood state (measured with SWEWBS/ONS4 Happiness Pulse); physical / clinical health metrics can be better utilised to measure improvements in co-occurring health conditions.

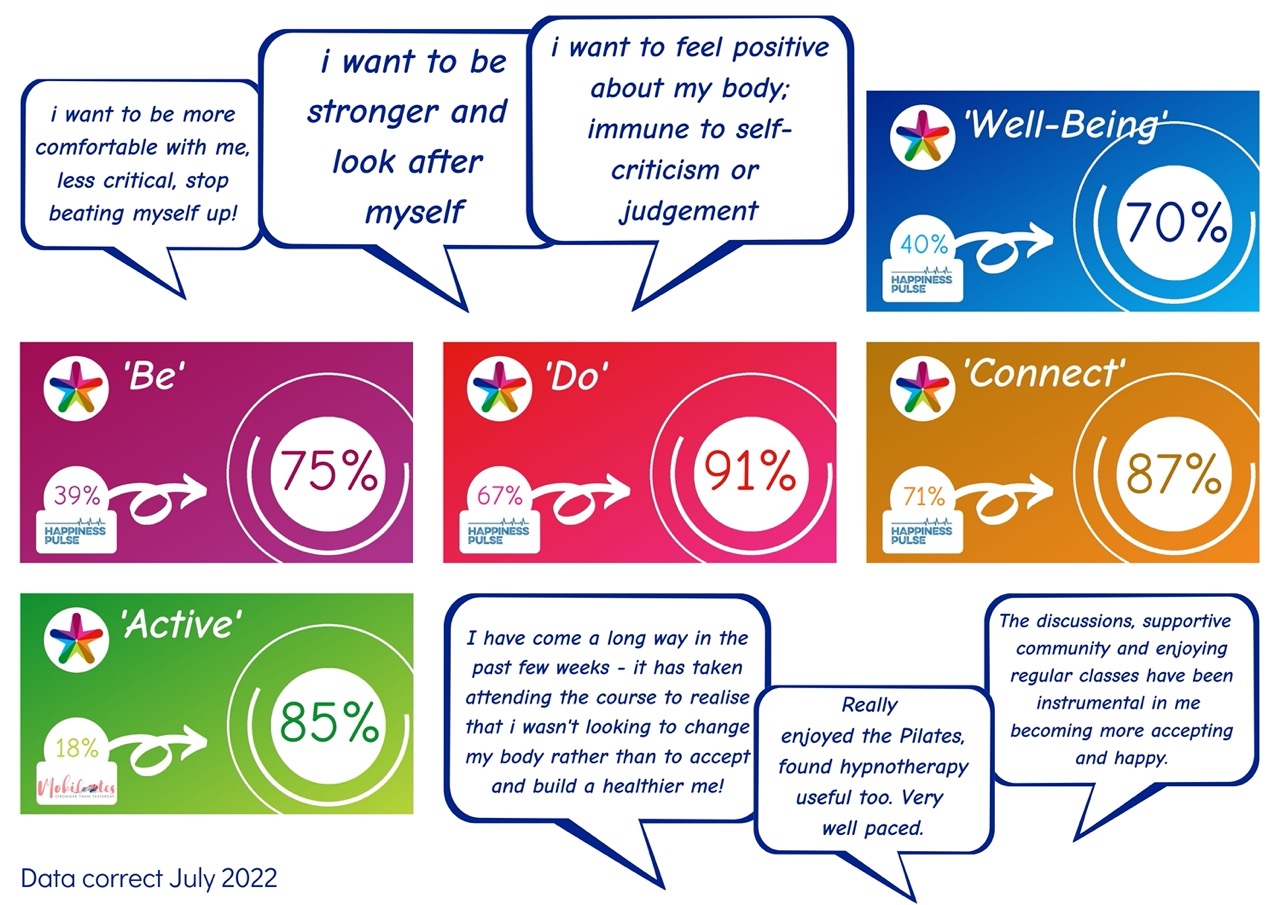
During our pilots for Weight Neutral Training and Food & Body Ease we use Thriving Places Happiness Pulse which incorporates ONS4 and SWEWBS - overall we’ve measured;
General Wellbeing 40% increased to 70%
‘BE’ 39% increased to 75%
‘DO’ 67% increased to 91%
‘CONNECT’ 71% increased to 87%
A collaboration with an accessible pilates provider, Mobilates, also measured ‘ACTIVE’ 18% increased to 85% sustained.
Traditional ‘weight focused’ interventions have very low engagement and completion rates. Data from OHID for 2021 Weight Management Services showed Dr referrals who complete at 8% and self referrals who complete at 12% - in comparison VCSE Nutriri’s services hold an 80-100% engagement and completion rate.
A schools based ‘body image’ workshop with 120 teenagers, using emoji feedback, measured increases in worthiness / acceptance / optimism - and reductions in low mood / detachment / body anxiety.
“I want to be stronger and look after myself”
“I want to be more comfortable with myself, less critical, stop beating myself up!”
“I want to feel positive about my body, immune to self-criticism or judgement”
“The discussions, supportive community and enjoying regular classes have been instrumental in me becoming more accepting and happy”
“I have come a long way in the past few weeks, it has taken attending the course to realise that i wasn’t looking to change my body rather than to accept and build a healthier me”
*
We can help existing services to refine their messaging and demonstrate that they are contributing to knowledge mobilisation and large scale change. With bias awareness training alongside improving ‘weight neutral’ access, encompassing physical activity, balanced nutrition, unpressurised alcohol and cigarette reduction, offering a comprehensive approach to improving public health, independent of weight change.
By addressing the underlying social determinants of health, fostering inclusive communities, and empowering individuals to make informed choices about their whole health, we can help create a society where everyone has more opportunity to thrive.